Three million Ohioans on Medicaid face major coverage changes beginning this August 1.
Most will be eligible for less expensive dental and vision coverage. State numbers show 12,483 people could lose their Medicaid dental and vision coverage.
Some of those people tell 10 Investigates they did not know about the potential of losing their coverage until last week.
Marion resident Brittini Peck is on Ohio disability after four open heart surgeries for a congenital defect. She gets medical coverage through Medicare and could get dental and vision coverage through Ohio Medicaid.
Currently, Peck receives $1,179 a month on disability. She pays $642 a month for rent and utilities. Ohio won’t pay for dental or vision coverage unless Peck spends $516 of her own money each month as a deductible. That deductible is called a “spend down.”
“There's no way I could have afforded to meet that spend down, but to find out there was no way I was ever going to have that as an option, that was a shocker,” Peck said.
Last week, when a county caseworker told her those deductibles were ending August 1, Peck thought it was good news. However, disabled people like Peck who are on Medicare stand to lose their dental and vision coverage.
According to the Ohio Job and Family Services Directors’ Association, those with income, including disability payments totaling between 75 to 138 percent of the Federal Poverty Level, will lose their Medicaid dental and vision coverage.
Since Peck receives Medicare that provides no dental or vision coverage, she is ineligible to receive coverage through the Affordable Care Act exchange that would provide dental and vision coverage. For Peck and her heart condition, dental coverage is a necessity.
"If I get an infection, one of those bad cavities, it could lead to bacterial endocarditis in my heart. And that would be very deadly. I've already had it once," Peck said.
"At the end of the day, at some point over the next 18 months, there are individuals who are going to lose health care as a result of this policy change. I certainly wish we had done more,” Joel Potts, president of the Ohio Job and Family Services Directors’ Association, said. “This has been a very confusing system. It is a major change and we're really not sure how many people fit in that category.”
Sources tell 10 Investigates the state did not give complete lists to Ohio counties trying to notify those losing their Medicaid coverage.
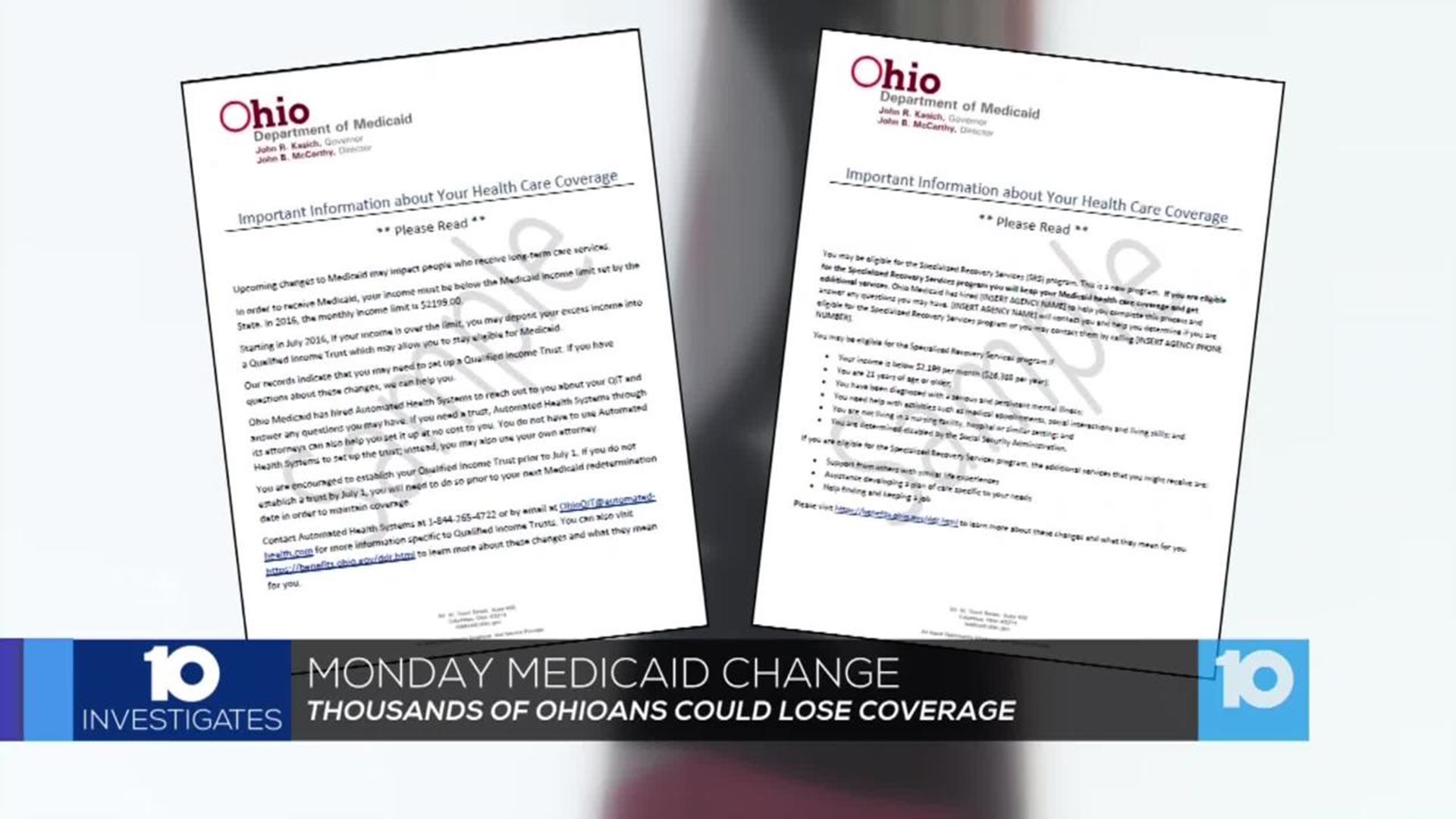
The state said they sent out notices to Medicaid recipients. 10 Investigates asked the state Medicaid department for proof and to provide copies of those notices.
The department gave 10TV two forms they sent to over 15,000 people , but Peck and county agencies say they simply didn't get them.
Ohio's Medicaid Department declined an interview, releasing the following statement:
“Ohio is joining the majority of states in simplifying the disability benefit eligibility process and increasing the benefit income limit for aged, blind and disabled citizens. Individuals directly impacted by program changes have been mailed information, and Ohio Medicaid has worked closely with County
Departments of Job and Family Services and advocacy groups to communicate program changes, as well. We will continue to work with our partners to assist any constituents who need help understanding, applying for or receiving benefits. Unfortunately, with this specific case, inaccurate information shared at the local level led to a misunderstanding of benefits eligibility and program changes. However, once Ohio Medicaid was made aware of the situation, we worked with the county to resolve the case.”
OJFSDA tells 10 Investigates that county agencies will be able to help Medicaid recipients past the August 1 deadline.
County agencies can offer 18 months of transitionary Medicaid coverage to those not eligible for the August 1 program changes.
Those Medicaid recipients may need past medical receipts from this past year to be eligible for the temporary Medicaid extension.
OJSDA recommends calling your local county Job and Family Service agencies as soon as possible for additional information on Medicaid eligibility:
- Franklin County: (614) 233-2000
- Delaware County: (740) 833-2300
- Licking County: (740) 670-8999
- Fairfield County: (740) 652-7889
- Pickaway County: (740) 474-7588
- Madison County: (740) 852-4770
- Union County: (937) 644-1010